Hip Services
Services offered by:
Mr. Brad Crick, Mr. Peter Hamilton, Mr. Peter McCombe, Mr. Richard Large
-
Revision Total Hip Replacement
Revision Total Hip Replacement
Indications
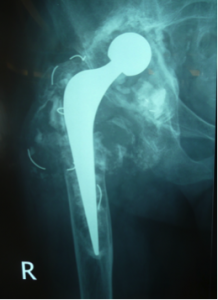
Total Hip Replacements(THR) usually perform particularly well in the long term. In fact, according to the Australian Joint Registry, over 95 % of THR’s are still functioning well at the 10 year mark and many function well for much longer.However, sometimes hip replacements can run into trouble and repeat surgery, Revision Total Hip Replacement( Rev THR), is needed. This can involve either just the cup side or the femoral side of the replacement or both.
The commonest cause of failure is when the components lose their fixation to the bone – loosening. This more commonly affects the cup and is usually due to wear of the surface of the component. Sometimes the wearing process can lead to bone loss (lysis) without loosening. Other, less common indications for Rev THR include multiple dislocations, infection and fracture around the femoral stem of the replacement.
Sometimes in THR where a metal surface rubs against metal, there can be tissue reactions against the metal particles
Relevant Investigations
XRays are the most important investigation in a troublesome THR. Regular monitoring of patients with THR is important. The frequency of review varies with surgeon preferences, prosthesis type and duration since surgery.XRays help to diagnose loosening and lysis and can help in cases of dislocation and fracture. Blood tests to exclude infection and check metal levels are useful and CT scan, Bone Scan, Ultrasound and occasionally MRI can be very helpful.
Procedure
Rev THR usually has 2 aspects to the surgery. The first is to remove the troublesome prosthesis or prostheses. This can be easy( eg in a very loose cup) or sometimes extremely difficult ( eg in a well fixed femoral stem with incorrect orientation).After removing the prostheses, the second aspect of the operation is to insert new components. Again this can be straightforward or complex. If there has been a lot of bone loss, then bone graft may be needed and components with more metal may be used. Sometimes, in extreme circumstances, individual 3D printed prostheses based on CT scans can be employed to replace large areas of bone loss.
In infection, these 2 stages will usually be separated so that the prostheses are removed in the first procedure and then, some weeks later, the new prostheses are inserted after appropriate antibiotic treatment.
Rehabilitation
Recovery from Rev THR is usually very similar to primary(first time) THR. Mostly patients can weight bear as able. Occasionally, when bone graft has been used or if the prosthesis only has a delicate grip on the bone, then there may be a 6 or 12 week period of restricted weight bearing.The risks of Rev THR are similar to THR with infection, thrombosis, dislocation, fracture and nerve injury always a concern. Of these, dislocation and infection may be slightly more common than in primary THR, especially in more complex surgery.
Revision THR is usually extremely successful and the longevity of the replacement approaches the same rates as primary THR with 90% still functioning well at 10 years after operation
-
Total Hip Replacement
Total Hip Replacement
Introduction
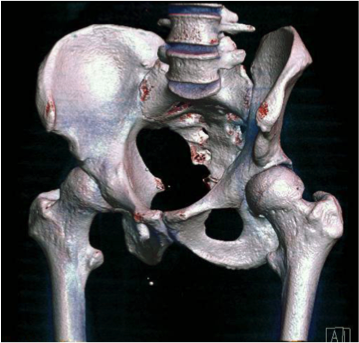
The hip is a ball and socket joint and is subject to a number of conditions that may cause the joint to wear out. If symptoms are minimal then simple painkillers and lifestyle modification may be all that is required to function well, but if symptoms become severe enough to affect your quality of life then surgery to replace the joint may be considered.
Investigations
A plain xray is often all that is required to make the diagnosis of osteoarthritis. At times further tests may be required also.
Procedure Synopsis
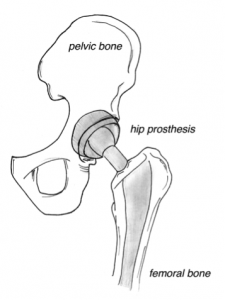
Total Hip Replacement involves surgery to dissect down to the hip joint. There are a few different methods for this dissection, which your surgeon will be happy to discuss. The ball at the top of the femur (femoral head) is then removed and the femur and socket (acetabulum) is shaped to allow a new hip prosthesis to be placed. The prosthesis is then positioned in the femur and the acetabulum to reconstruct a new artificial ball and socket.
Rehabilitation
Patients should expect that they will have some pain while recovering from surgery. Most patients will stand a day or two after surgery and begin walking with the assistance of a frame and gradually proceed to using crutches. The length of time in hospital is variable but most patients can go home or to rehabilitation after 5-7 days.
In the initial stages after a hip replacement, your surgeon is likely to restrict your activities in order to protect against dislocation. Most of these restrictions will be able to be relaxed after six weeks.
Full recovery after a joint replacement can be up to 6-12 months, but most patients experience very few issues after the initial 6 weeks.
Special considerations
Various different bearing surfaces and prosthesis types can be considered. Hip replacements typically should last for at least 10-15 years but as with any mechanical device they can eventually wear out and may require revision surgery.
-
Hip Arthroscopy
Hip Arthroscopy
Introduction
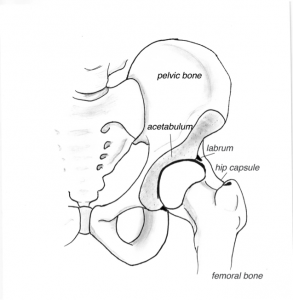
Hip arthroscopy is a procedure often performed by orthopaedic surgeons to diagnose and treat various causes of hip pain. It allows good visualization of the sufaces of the hip joint and surrounding muscles and other structures.
Common reasons for a hip arthroscopy may be to treat a tear in the labrum (rubber-like seal around the hip joint), remove loose bodies or remove a bone prominence that is causing impingement of the joint.
Investigations
A plain xray is usually the first investigation for hip pain. Other investigations such as an MRI will show a more detailed view of the soft tissues and internal structure of bone, cartilage, muscles and soft tissue around the hip. Unfortunately these tests can also sometimes detect things that may not be causing symptoms due to their high sensitivity.
Often the treating surgeon will consider a hip injection to prove the source of the pain prior to considering surgical options. Other imaging such as CT may also be required.
Procedure Synopsis
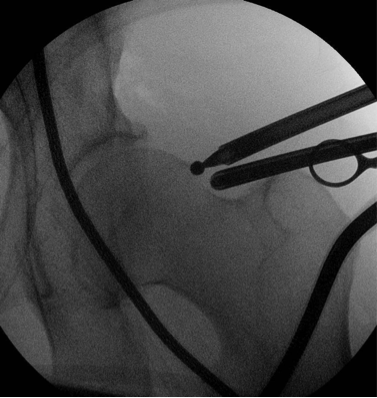
Hip Arthroscopy involves surgery place a telescope into the hip joint to directly visualize the surfaces and surrounding structures. The hip joint does not usually have any space between the ball and socket, and hence a special table is usually required to place traction on the leg. The traction device pulls the ball out of the socket a small distance to allow room for the instruments to get into the hip joint. After the ball and socket have been assessed and treated, the traction is released to allow the ball to return into its normal position in the socket.
The peripheral compartment of the hip can also be assessed. If a bone prominence on the neck of the femur is causing impingement of the joint then this can be removed with various other tools.
Rehabilitation
Patients should expect that they will have some pain while recovering from surgery. Most patients will be able to stand and walk after surgery and do not always require crutches. In certain circumstances, the surgeon may need to limit your movement and may impose some restrictions. Most patients will need to stay overnight in hospital but some may be able to leave on the same day.
Driving is possible once the hip feels comfortable but often best avoided for at least the first 48 hours.
Results of hip arthroscopy are often improved with physiotherapy. Your surgeon will advise when physiotherapy can commence and guide your rehabilitation program.
Full recovery after a hip arthroscopy can be up to 3 months.
Special considerations
As with any surgery, hip arthroscopy does carry some risk. In rare circumstances, the traction that is required can disturb the blood flow to the femoral head and cause a condition called avascular necrosis. Nerve injuries and damage to the articular surface of the hip can also occur. Despite the highest standards of care, complications are possible.
-
Direct Anterior Approach Hip replacement
Direct Anterior Approach Hip replacement
The DAA is a minimally invasive technique that offers many advantages with early post-operative recovery. This is attributed to the fact that an anterior incision does not significantly disrupt the muscles and tendons like the more traditional lateral or posterior approach to hip replacement.
While you are in hospital, the nursing team, together with your Physician(if you need one), Physiotherapist and Orthopaedic surgeon will work with you on an individualised plan of care. This includes minimising any post- operative complications with compression stockings, a spirometer to assist you with respiratory function if required, and the administration of appropriate medications to ensure you are free from pain/discomfort. You will be encouraged to be up and out of bed the day after your surgery.You will find you are ready to go home after 3 days. If you live by yourself, it may be possible to remain in hospital for an extra day or two if you need to. The DAA technique allows patients to go home directly from hospital and avoids the need of an admission to a rehabilitation facility. You will have some exercises to do once you go home to assist your muscles in remaining toned so that your body can adjust to your new hip.
The DAA approach means you DO NOT need to worry about the usual precautions required with lateral/posterior hip replacements. You can sleep in any position that is comfortable, you do not need to worry about crossing your legs or excessive rotation/bending restrictions.
Please call the office on 5976 0877 for more information.