Shoulder Services
Services offered by:
Mr. Richard Large, Mr. Andrew Weber
-
Total Joint Replacements
TOTAL JOINT REPLACEMENTS
Mr. Andrew Weber & Mr. Richard Large
Introduction
For over 100 years surgeons have been improving joint replacements to the stage where we almost take it for granted. Joint replacements became reliable during the 60’s when Sir John Charnley revolutionised the total hip replacement. Now patient’s can look forward to virtual pain free movement for many years. While hip replacements and knee replacements are common, shoulder replacements are now also routine. Joint replacements however, should not be looked upon as being as good as the original, and there are a number of factors to consider.Indications
A shoulder replacement is indicated for arthritis, whether that be osteoarthritis, rheumatoid arthritis or post traumatic arthritis. The type of shoulder replacement will depend on the pathology, that is the state of the rotator cuff around the shoulder, and possible wear of the bone involved in the arthritis.Relevant Investigations
X-ray and ultrasound are standard investigations for shoulders. A CT in a shoulder replacement is often used to assess the alignment of the scapular and the amount of bone the surgeon has to work with.Procedure Synopsis
With a shoulder replacement, an incision is made down the front of the shoulder. Surgical dissection is made between the deltoid and pectoralis major muscles. The subscapularis, the muscle in front, needs to be elevated to expose the shoulder. The components are fixed to scapular and humerus through this space. How they are fixed will again be dependant on the pathology.Rehabilitation
The patient will awake with a drain coming from their arm, in a sling. The arm will be immobilised for approximately six weeks. It is very important that the muscles heal around the joint replacement for its long term viability, stability and function.
You will leave hospital with some waterproof dressings on your wounds. Please leave these dressings intact until your post operative visit at one week post op. You will be prescribed some pain medication, and it is recommended that you take this regularly to stay on top of your pain.
You will be seen by the hospital physiotherapist who will show you a home exercise program prior leaving hospital. Gentle pendular exercises for your shoulder can be commenced straight after the surgery. Do not lift anything more than a coffee cup for the first six weeks after surgery.
These are the range of motion exercises to be performed immediately after the surgery:
WEEKS 1 to WEEK 6:
- Wear sling at all times including in bed
- Wear shower sling for washing
Exercise program
WEEKS 6 to WEEK 12:
- Regain range of motion of the shoulder
WEEK 13 +:
- Regain strength
There is always associated muscle wasting, and so it takes some time to regain the normal strength coordination required for the complex movement of a shoulder joint.
Joint replacements usually require regular review over the following years to assess for any signs of loosening.
Complications
Any operative procedure has potential complications. These will be discussed fully with you at the consultation.
-
Shoulder Instability
SHOULDER INSTABILITY
Mr. Andrew Weber & Mr. Richard Large
Indications
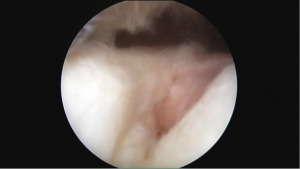
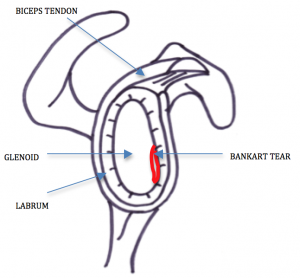
The shoulder joint is a highly mobile joint that allows you to lift your arm above your head and reach behind your back. As a result of having such a large range of motion, shoulder instability is common. Instability occurs when the humeral head (or ball) is forced out of the glenoid (or socket). This can happen as the result of trauma or from a repetitive overuse injury. If it occurs traumatically in a young athlete, surgery is often recommended to prevent re-dislocation, but an older person with an overuse injury may be better managed conservatively in the first instance.Usually the shoulder subluxes or dislocates in a certain direction (see the picture below). The shoulder capsule, ligaments and muscular system work in combination to ensure that the normal shoulder works effectively. These may be damaged (loose or torn) with a dislocation and thus repeat dislocations may occur.
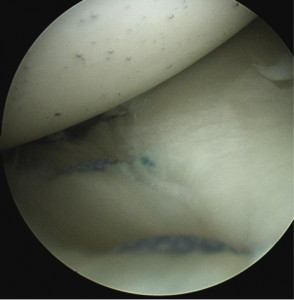
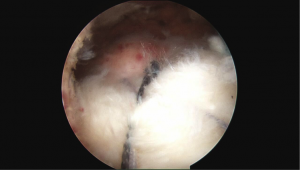
When the shoulder dislocates anteriorly (out the front), the labrum (the cartilage rim around the edge of the glenoid) may tear. This is known as a Bankart lesion.
Some individuals are predisposed to multi-directional instability. This is a difficult problem to manage, and individualised management is best discussed with your surgeon.
The acromioclavicular joint (or AC joint) is the joint between the acromion of the scapula (shoulder blade) and the clavicle (or collar bone). AC joint instability is usually the result of trauma.
Relevant Investigations
X-ray and ultrasound are standard investigations for shoulders. An MRI is often used to ascertain the extent of the cartilage damage.Procedure synopsis
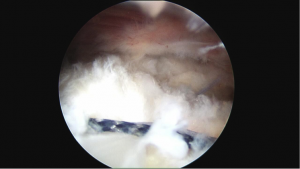
A shoulder arthroscopy is the most common surgical procedure used to treat shoulder instability (ie. an arthroscopic Bankart repair or Laterjet procedure).
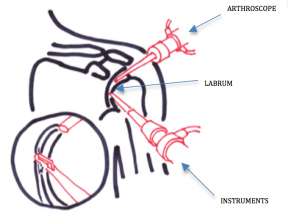
Stabilisation surgery involves 2 -4 small incisions made around the shoulder through which the arthroscope and instruments are inserted. These instruments are used to repair the cartilage, tendons and ligaments. Pictures of the operation can be taken during the procedure. When the operation is complete, the wounds are closed with a stitch and then covered with a waterproof dressing.The keyhole technique has some possible advantages compared with traditional methods of surgery using larger incisions:
- Less pain
- Shorter hospital stay
- Less stiffness following the surgery
- Better ability to identify and treat other areas of damage
Rehabilitation
You will leave hospital with some waterproof dressings on your wounds. Please leave these dressings intact until your post operative visit at one week post op. You will be prescribed some pain medication and it is recommended that you take this regularly to stay on top of your pain. You will be seen by the hospital physiotherapist who will show you a home exercise program prior to leaving hospital. Gentle pendular exercises for your shoulder can be commenced straight after the surgery. You should expect the shoulder to be painful although early movement will prevent stiffness. Do not lift anything more than a coffee cup for the first six weeks after surgery.
These are the range of motion exercises to be performed immediately after the surgery:
WEEKS 1 to WEEK 6:
- Wear sling at all times including in bed
- Wear shower sling for washing
WEEKS 7 to WEEK 12:
- Regain range of motion of the shoulder
WEEK 13 +:
- Regain strength
There is always associated muscle wasting, and so it takes some time to regain normal strength, and the coordination required for the complex movement of a shoulder joint.
Complications
Any operative procedure has potential complications. These will be discussed fully with you at the consultation.Videos
-
Rotator Cuff Injury
ROTATOR CUFF INJURY
Mr. Andrew Weber & Mr. Richard Large
Introduction
The shoulder joint is a complex joint that requires several structures including the rotator cuff muscles to work in a co-ordinated manner to provide a stable fulcrum for your arm to rotate. With this complexity, and the spectrum of different possible injuries, this summary below can only be generalisationCuff injuries are classified as either partial, or full thickness tears. They may the result of degeneration where the tendon progressively wears out. Acute trauma may also cause rotator cuff tears, and these may be associated with other injuries around the shoulder.
Indications
Indications for surgery are individualised for the extent of any tearing, the age, activity level, general health and expectations of the individual patient. A partial tear or simple impingement, or a full thickness tear at a later age, may be able to be treated with conservative management such as a number of cortisone injections and a rotator cuff strengthening programme, supervised by a physiotherapist. As a generalization the older we get the more likely we are to wear through a rotator cuff and therefore, as it is a normal part of aging as one gets older, a repair becomes more optional. We will assess each case and discuss the options with each individual patient to work towards the best option for them.Relevant Investigations
We like to assess the soft tissues, such as, the tendons and muscles, as well as the bone. An ultrasound covers the soft tissues and an X-ray gives us an idea of the bone. An MRI can assess both.Procedure Synopsis
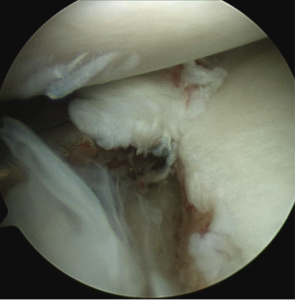
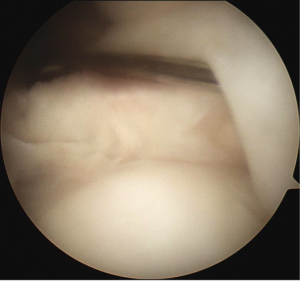
There is a myriad of different possible injuries associated with the rotator cuff. The most common though is a small full thickness tear of the supraspinatus tendon. Normally surgery is undertaken, at least initially, arthroscopically, that is through a telescope. We look into the shoulder and assess the extent and nature of the problem. Shaving of the bone may be indicated to treat any impingement. Attention to the biceps tendon that runs through the shoulder, or the cartilage in the shoulder may also be warranted depending on the pathology. Then the rotator cuff is examined and maybe repaired through the telescope, or less commonly these days, a small open approach may be required.Rehabilitation
Most patients would spend one night in hospital and go home in a sling, if a repair is performed. While we can sew a tendon back to bone, your body needs to heal it, which means up to six weeks in a sling. Shoulder surgery can be painful, however we are much better these days keeping the pain under control.You will leave hospital with some waterproof dressings on your wounds. Please leave these dressings intact until your post operative visit at one week post op. You will be prescribed some pain medication and it is recommended that you take this regularly to stay on top of your pain. You will be seen by the hospital physiotherapist who will show you a home exercise program prior to your discharge from hospital. Gentle pendular exercises for your shoulder can be commenced straight after the surgery. You should expect the shoulder to be painful although early movement will prevent stiffness. Do not lift anything more than a coffee cup for the first six weeks after surgery.
These are the range of motion exercises to be performed immediately after the surgery:
WEEKS 1 to WEEK 6:
Wear sling at all times including in bed
Allowed to remove sling for showers (let arm hang by your side only)
WEEKS 7 to WEEK 12:
Regain range of motion of the shoulder
WEEK 13 +:
Regain strength
There is always associated muscle wasting, and so it takes some time to regain normal strength, and the coordination required for the complex movement of a shoulder joint.
Complications
Any operative procedure has potential complications. These will be discussed fully with you at the consultation. -
Shoulder Impingement
SHOULDER IMPINGEMENT
Mr. Andrew Weber & Mr. Richard Large
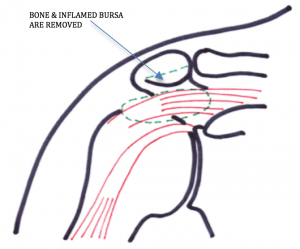
Indications
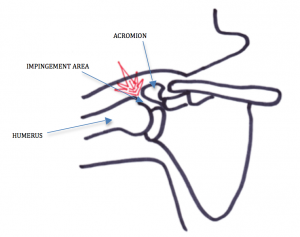
Shoulder impingement is a painful condition caused by the pinching of the rotator cuff tendons under the bone at the point of the shoulder. Pain may restrict the ability to raise the arm.
Relevant Investigations
X-ray and ultrasound are standard investigations for shoulders. An MRI is often used to ascertain the extent of the soft tissue damage.Procedure Synopsis
If conservative measures are not successful, a subacromial decompression may be recommended. This arthroscopic surgical procedure involves shaving a portion of the bone from the acromion. Bone spurs are also removed if present, and the bursa resected if it is thickened and inflamed. It may also be necessary to repair the rotator cuff tear.
The keyhole technique has some possible advantages compared with traditional methods of “open” surgery using larger incisions:
- Less pain
- Shorter hospital stay
- Less stiffness following the surgery
- Lower chance of infection
- Better ability to identify and treat other areas of damage
Rehabilitation
A subacromial decompression alone imposes very few restrictions post operatively. You will be provided with range of motion exercises on Day 1 after the operation. The shoulder will be painful in the first few days, but this will gradually reduce. It is normal to feel discomfort when lifting items or raising the shoulder high for the first 6 to 8 weeks. Full recovery is from 4 to 6 months. There will be no restrictions imposed on what you can do with the arm during the recovery period, within the limits of pain. General advice however is not to “stress” the shoulder with heavy lifting or repetitive overhead tasks within the first 2 to 3 months to allow the best chance for good recovery. Don’t do too much too soon.
If combined with a rotator cuff tear, you will be more restricted post surgery (see page on Rotator Cuff).
There is always associated muscle wasting, and so it takes some time to regain normal strength, and the coordination required for the complex movement of a shoulder joint.
Complications
Any operative procedure has potential complications. These will be discussed fully with you at the consultation.Videos:
-
Frozen Shoulder / Adhesive Capsulitis
FROZEN SHOULDER / ADHESIVE CAPSULITIS
Mr. Andrew Weber & Mr. Richard Large
Natural history
A frozen shoulder or adhesive capsulitis is a significant inflammatory response that may be secondary to trauma, but often can just start with no precipitating event. For reasons that are poorly understood, the capsule inside the rotator cuff of your shoulder has become very inflamed and as a result, scarred down and thickened. The natural history of a “frozen shoulder”, without treatment, is usually approximately 6 months of pain, and 18 months of stiffness. Things then usually slowly resolve leaving the patient with a normal, or near normal range of movement. There may be an underlying cause such as impingement, rotator cuff or cartilage problems that led to the frozen shoulder in the first place. There is a small chance of these requiring attention later. Surgery is usually avoided during the early course of a frozen shoulder, as any further stimulus will simply make the inflammation worse.Diagnosis
The diagnosis of a frozen shoulder/adhesive capsulitis is largely clinical by examination. The most common restriction is that of external rotation, that is how much the forarm can rotate outwards with the arm by the side. An ultrasound can be helpful to assess any rotator cuff pathology, and an X-ray useful, as the other entity that can cause similar symptoms is arthritis, which is easily determined up by having and X-ray or MRI.Management
(Conservative)Management is usually conservative, that is without surgery. This can be directed by a general practitioner, sports physician, rheumatologist or orthopeadic surgeon. In the very acute, painful stage, a cortisone injection into the shoulder proper may alter the severity. It is important that the shoulder is not hurt more, and as such we would caution against any forceful manipulation, or any excessive activity that provokes more discomfort. Pain medication is useful, and anti-inflammatories can be tried. Physiotherapy can assist with a gentle home stretching program, and working on posture. As your movement improves later, you will require a lot more physiotherapy to regain normal shoulder strength.
The next step is injection into the shoulder of local anaesthetic and cortisone. This may also be combined with saline, known as a hydrodilatation.
Under X-ray control the radiologists insert a needle into the shoulder joint, inject local anaesthetic and cortisone and then distend the shoulder joint with normal saline fluid, to create more space and hence range of movement. While local anaesthetic is inserted, this still involves a needle and the distension of the joint leads to pain at the time. During insertion of the needle the X-ray machine is placed close to your face in order to provide guidance and placement of the needle. There may be some discomfort for 48 hours afterwards, but most of the pain is during the procedure. The aim of this is to help the pain you’re experiencing every day. Truthfully, none of the options listed above give a simple, quick, easy cure. The inflammatory process usually still persists over many months. The purpose of the procedure, such as an injection, is to make the symptoms and stiffness more tolerable.
(Operative)
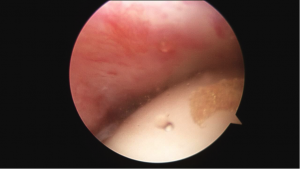
Further procedures are sometimes required for more severe cases. An arthroscopy can be performed to debride the inflammatory tissue and release the tight capsule. This is usually performed after the acute inflammed period.
Rehabilitation
Following a hydrodilitation or surgery, physiotherapy is recommended to regain range of motion and improve function. -
Slap Tears
SLAP TEARS
Mr. Andrew Weber & Mr. Richard Large
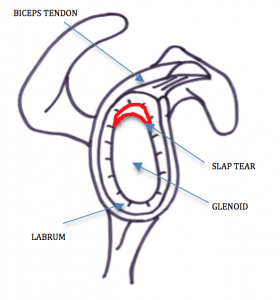
Indications
A SLAP lesion (Superior Labrum, Anterior to Posterior) occurs when the top portion of the labrum is damaged. As this is the site of the biceps tendon attachment this can also be involved in the injury. Injuries to the superior labrum can be a result of acute trauma, or by repetitive shoulder motion. SLAP tears are commonly seen a normal part of the aging process. In older patients more conservative treatment may be indicated. This will be discussed with your surgeon after assessment.The SLAP lesion can cause pain in the shoulder, catching/clicking/clunking with movement, impingement or “pinching” of the rotator cuff tendons when lifting the arm.
Relevant Investigations
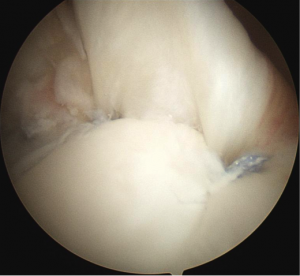
X-ray and ultrasound are standard investigations for shoulders. An MRI is often used to ascertain the extent of the soft tissue damage.Procedure Synopsis
SLAP lesions do not generally heal by themselves. Surgery may be necessary and involves arthroscopic repair of the labrum and biceps tendon with suture anchors. The keyhole technique has some possible advantages compared with traditional methods of “open” surgery using larger incisions:- Less pain
- Shorter hospital stay
- Less stiffness following the surgery
- Lower chance of infection
- Better ability to identify and treat other areas of damage
Rehabilitation
You will leave hospital with some waterproof dressings on your wounds. Please leave these dressings intact until your post operative visit at one week. You will be prescribed some pain medication, and it is recommended that you take this regularly to stay on top of your pain. You will be seen by the hospital physiotherapist who will show you a home exercise program, prior leaving hospital. Gentle pendular exercises for your shoulder can be commenced straight after the surgery. You should expect the shoulder to be painful although some gentle early movement will prevent stiffness. Do not lift anything more than a coffee cup for the first six weeks after surgery.
These are the range of motion exercises to be performed immediately after the surgery:
WEEKS 1 to WEEK 4
Wear sling at all times including in bed
Allowed to remove sling for showers (let arm hang by your side only)
WEEKS 5 – 6
Do not externally rotated your arm
WEEK 7 – 12
Regain range of motion of the shoulder
WEEK 13 +
Regain strengthThere is always associated muscle wasting, and so it takes some time to regain normal strength and coordination required for the complex movement of a shoulder joint.
Complications
Any operative procedure has potential complications. These will be discussed fully with you at the consultation. -
Fracture of Upper Limb
FRACTURE OF UPPER LIMB
Mr. Andrew Weber & Mr. Richard Large
Indications
Many fractures in the upper limb can be managed conservatively either in a plaster or a sling. Fractures (broken bones) that are minimally displaced, well aligned and closed usually heal well without the need for surgery.Relevant Investigations
X-rays provide the most relevant information required to determine the best management of fractures of the upper limb. Sometimes more detailed scans are required to assist with management planning.Procedure synopsis
Fractures of the humerus can be managed surgically with a plate and screws, a humeral nail or in more severe fractures of the humeral head may require a shoulder joint replacement. Fractures of the scapula (shoulder blade) can generally be managed without the need for surgery. Most clavicle fractures can be treated without surgery. Surgery is necessary for clavicle fractures that are severely displaced, about to break through the skin, or fractures at the lateral end. These procedures are done under general anaesthetic and usually require a short stay in hospital.Rehabilitation
Bone healing can take up to twelve weeks. After six weeks the fracture is usually strong enough to be taken out of a sling. It is usually advised to wait for return to heavy lifting, weight bearing and contact sports until twelve weeks after injury.Complications
Any operative procedure has potential complications. These will be discussed fully with you at the consultation.